The Truth About Common Digestive Health Fears

Everyone experiences digestive problems now and then, and they’re nobody’s idea of a good time. In a survey of nearly 72,000 adults in the U.S., 61% reported having had at least one gastrointestinal (GI) symptom over the previous week, and within that group, 58% said they’d had two or more GI symptoms over the past week, according to a study in a 2018 issue of the American Journal of Gastroenterology Because symptoms like constipation, heartburn, and abdominal pain are generally vague and often don’t have an obvious cause, those suffering tend to fear the worst.
“People get very concerned about GI symptoms—they often worry that there is something serious going on, such as cancer,” says Dr. Byron Vaughn, an associate professor of medicine and co-director of the IBD program at the University of Minnesota in Minneapolis. “Because it’s not socially acceptable to talk about GI illnesses at cocktail parties or other social gatherings, people don’t get social support, and they end up thinking about their symptoms more and more.”
[time-brightcove not-tgx=”true”]
In many cases, this can increase stress and cause digestive distress. And for those who have irritable bowel syndrome (IBS)—a disorder characterized by abdominal pain along with changes in bowel habits (such as constipation, diarrhea, or alternating bouts of the two)—fears about symptom flare-ups can take a toll on emotional well-being and quality of life, research has found. In fact, there’s evidence that patients with IBS have a higher prevalence of depression and lower quality of life than those who don’t have the condition. Also, overall happiness tends to decrease.
To sidestep unnecessary stress and worry, it’s time to give common concerns related to digestive health a reality check. Continue reading to learn more about the most common fears gastroenterologists receive from patients.
This is the fear Colon cancer is more likely if you suffer from constipation.
Here are some factsThe idea that colon cancer risk could rise if it was exposed to toxic or potentially carcinogenic substances from feces for a prolonged period of time used to be popular. However, studies do not support this notion. “There’s no added risk of colon cancer with constipation—they’re two totally separate issues,” Vaughn says. “Transit time doesn’t matter” as far as the risk of colon cancer goes. Constipation, which affects around 16% of American adults and 33% of older Americans, is very common. There are many definitions of constipation. Some people experience multiple bowel movements per day, while others only have one or two. The American Gastroenterological Association describes constipation as having three or fewer bowel movements each week, and hard-to pass bowel movements.
By contrast, risk factors for colorectal cancer include a diet high in red meats, smoked foods, and processed foods; smoking; moderate to heavy alcohol consumption; lack of regular physical activity; obesity; inflammatory bowel disease such as Crohn’s disease or ulcerative colitis; and a family history of colorectal cancer. The U.S. Preventive Services Task Force lowered from 50 the average age to screen for colorectal carcinoma in order to reduce the incidence among young adults.
This is the fearStress is a cause of ulcers
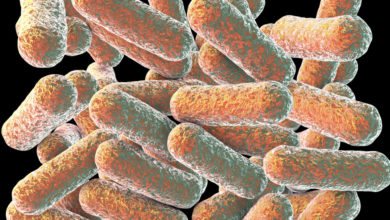
Here are some facts The most common causes of peptic ulcers—which are sores on the lining of the stomach or duodenum (the first part of the small intestine)—are long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, ketoprofen and aspirin, or infection with the bacterium Helicobacter pylori (H. pylori). “Ulcers are due to a breakdown in prostaglandin synthesis, which affects the mucosal protective barrier, which is like acid-proofing for the stomach lining,” explains Dr. Christine Lee, a gastroenterologist at the Cleveland Clinic. “NSAIDs decrease the body’s ability to produce prostaglandins.” By contrast, H. pyloriBacteria can cause damage to the mucous layer, which allows stomach acid into the stomach or duodenum. Researchers have found that NSAIDs may cause a synergistic effect when used for prolonged periods. H. pyloriNSAIDs alone can lead to ulcers developing earlier than if there is an infection. Depending on the cause of a peptic ulcer, your doctor may prescribe different medications—such as proton pump inhibitors, histamine receptor blockers, or protectants—to relieve pain.
None of this means stress can’t cause stomach distress, however. Vaughn says that stress can lead to indigestion (or dyspepsia) and a burning, gnawing feeling. The symptoms may feel similar to ulcer discomfort, but they don’t stem from an actual ulcer.
This is the fear Having frequent diarrhea signals ulcerative colitis or Crohn’s disease
Here are some facts Rather than suggesting you have one of these inflammatory bowel diseases, it’s more likely that frequent diarrhea episodes stem from some type of food sensitivity, irritable bowel syndrome or medication side effects, says Dr. Shaham Mumtaz, a gastroenterologist at the Northwestern Medicine Regional Medical Group in the Chicago area. On the food front, “some types of foods pull more fluid into the gut and can cause bloating and diarrhea,” Mumtaz explains. “Some people are more sensitive to them than others are.”
In particular, foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs)—which are short-chain carbohydrates or sugars—can be problematic for people with IBS or small-intestinal bacterial overgrowth. FODMAP-rich foods include dairy, wheat, legumes and lentils as well as some fruits like apples and mangoes. They also contain artificial sweeteners and certain vegetables such as asparagus, broccoli and brussels sprouts. A study found that people who suffer from IBS and frequent diarrhea could eat a low FODMAP diet over four weeks to get adequate relief.
Red flags for ulcerative colitis or Crohn’s disease include unintended weight loss, changes in appetite, abdominal pain, bloody stools, fatigue, and persistent diarrhea for more than four weeks with lots of frequency and urgency, Mumtaz says. To diagnose inflammatory bowel disorders, a gastroenterologist should examine you. He may recommend an endoscopy (colonoscopy), imaging studies, and stool sample testing.
This is the fear Your risk of rectal cancer increases if you have hemorhoids
Here are some facts Hemorrhoids are swollen blood vessels in and around the anus and the lower rectum—they’re a bit like varicose veins—and they’re very common. The lining of both the anus and lower rectum are the places where internal hemorhoids occur, while the external form under the skin. “Take a good look with a mirror—they look like a bunch of grapes around the anus,” says Dr. Cindy Yoshida, a gastroenterologist and professor of medicine at the University of Virginia Health System in Charlottesville. They may itch too, and when they’re irritated, they can bleed when you wipe your bottom after a bowel movement. Here’s where things get tricky: “Bleeding from rectal cancer can be mistaken for bleeding from hemorrhoids—the bleeding can look the same on toilet paper,” Yoshida says. That’s why it’s important to always get rectal bleeding checked out by your doctor.
This is the fear If you go to the bathroom right after you eat, that means food is running through you and you’re not absorbing the nutrients
Here are some factsA few people may have an overactive gastrocolic reflex. This is a mechanism that regulates the flow of food through the lower gastrointestinal system after eating. For those with a particularly sensitive or heightened gastrocolic reflex—which can happen with irritable bowel syndrome—when they start eating and their stomachs start expanding, they get colonic spasms that lead to a bowel movement, Vaughn explains. What they actually pass isn’t the food that they just ate. It’s what was sitting in their colon, which means they’re still digesting and absorbing the food they just ate.
This is the fearSlow digestion can indicate a serious blockage
Here are some facts It’s probably a gut-motility issue, not an obstruction. “Think of the gut as a pipeline: if you have a blockage, things won’t go south,” Yoshida says. Which means they’re likely to travel north, leading to significant nausea and vomiting and a very distended or bloated belly. What’s more, says Dr. Seth Gross, a professor of medicine and clinical chief of the division of gastroenterology and hepatology at NYU Langone Health, “if you had a blockage, you probably wouldn’t be meeting me in the office because you’d be very sick. You can’t walk around that way.”
Truth is, as we get older our gut motility decreases. Also, certain medical conditions such as hypothyroidism or diabetes, as well as drugs like narcotic pain medication, may affect the speed at which food passes through the digestive tract. Yoshida suggests that you talk with your doctor if this is an ongoing issue. But if it’s something that’s been going on for a long time, it’s probably the result of your own naturally slow gut motility.
This is the fear Foul-smelling farts or poops signal that something’s wrong in your digestive tract
Here are some factsMany times, your food choices will influence the way you smell. “Based on what you feed your colon, you can make methane gas, hydrogen sulfide gas, carbon dioxide or ammonia,” Yoshida explains. In particular, she says, hydrogen sulfide gas—which stems from eating meat, eggs and fish—smells worse. Eating lots of cruciferous vegetables—such as broccoli, cabbage, and onions—can also increase the risk of bad-smelling gas or stools.
This is the fearYou should not see any food or other substances in your stool.
Here are some facts Seeing bits of undigested food in the toilet isn’t usually cause for concern, says Lee of the Cleveland Clinic. “Like life, your colon is not always respectful and orderly”—which is why particles of food can be visible in the toilet after a bowel movement. This can happen because some high-fiber foods—such as corn, carrots, nuts, seeds, and whole grains—“are not supposed to be broken down by the body, so we should expect that they will come out of the body intact,” Mumtaz says. This means that your high fiber diet is working. But in some cases undigested food particles can appear if you’re not chewing your food thoroughly.
It is normal to see undigested food particles in your stool. Gastroenterologists start to suspect a malabsorption issue when unintentional weight loss, fatigue, or weakness have occurred—and when stools look oily and are difficult to flush because they stick to the toilet, Mumtaz says. If your doctor is concerned, they’ll likely recommend a stool sample; blood tests to check for nutritional deficiencies or inflammation markers; an endoscopy to examine the upper digestive tract; or a colonoscopy to analyze the lower gastro-intestinal tract.
This is the fear Diverticulitis can be caused by eating nuts and seeds
Here are some factsDiverticulitis is a condition where small pouches within the digestive tract become inflamed. The theory was that nuts, seeds, berries, and other small bits of food could block pouches in the colon and lead to diverticulitis, Vaughn notes, but that’s been debunked. “Even if you have diverticulitis, you can eat these foods as long as you don’t feel bad after eating them,” he adds.
The exact causes of diverticulitis still aren’t understood. While it was long believed that a low-fiber diet and constipation could increase someone’s risk of developing diverticulitis—because of increased pressure within the digestive tract and straining during bowel movements—the latest research suggests otherwise. A study was published in the 2021 issue. Clinical Gastroenterology/Hepatology researchers tracked the health of participants in the Nurses’ Health Study for 24 years and found that those who had more than one bowel movement per day had a 30% greater likelihood of having diverticulitis, while those who had less than one BM per day were 11% less likely to have the condition.
This is the fearA hernia can be caused by lifting weights
Here are some facts This is admittedly a lie. A bulge beneath the skin is caused by an abdominal hernia, which occurs when part of an organ like the intestine pushes against a weakness within the abdominal wall. Any activity that involves bearing down—such as straining to poop because of constipation, persistent coughing or sneezing, or lifting heavy weights—or anything that increases intra-abdominal pressure, such as obesity and pregnancy, can increase your risk of developing an abdominal hernia.
But it’s not a sure thing. Plenty of people lift weights and don’t get hernias. “No one can predict who is at risk for developing a hernia,” Gross says. Some people may be born with one. Others might develop it because of an inborn weakness in the abdominal wall. Risk factors for this condition include previous abdominal surgery, smoking history, family history, or a family history with hernias.
The important thing is: “If you have a hernia, you should be mindful of putting pressure on that area,” Gross says. In other words, if you’ve been diagnosed with an abdominal hernia and you engage in heavy weight training or other strenuous forms of exercise, you could exacerbate the hernia or worsen its symptoms.